Student Research Spotlight
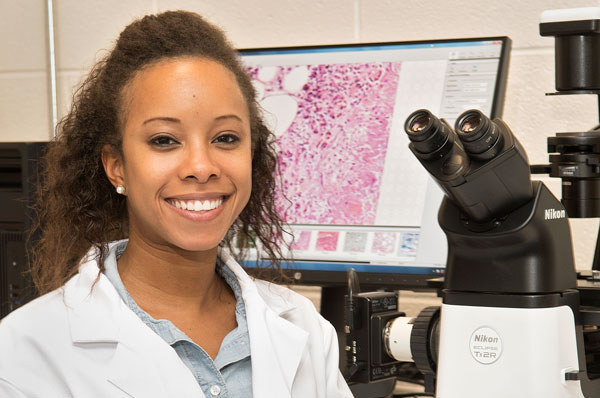
Arielle Roberts (DO ’21)
December 18, 2017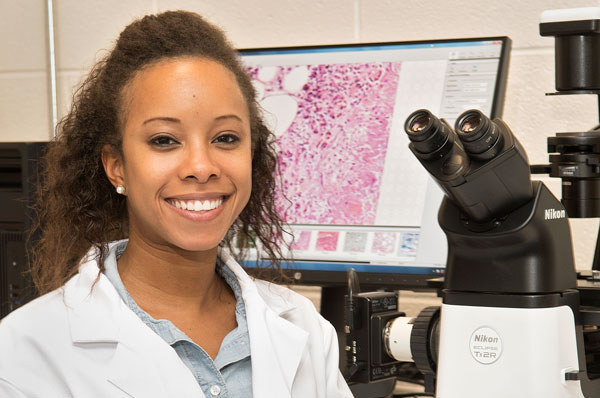
Roberts is working on research to help patients suffering from bladder and bowel incontinence
regain control.
Arielle Roberts (DO ’21) became interested in research upon completing her Master’s
thesis on pediatric obesity. She is interested in learning how laboratory discoveries
can help her future patients.
What did you study?
Under the guidance of Michael Ruggieri, PhD and Mary Barbe PhD, as a collaborative
team at Temple University School of Medicine, we studied methods to restore function
of the urinary bladder following a lower spinal cord injury using the canine model.
In addition, we also explored the morphological changes and pharmacological response
of the smooth muscle of the bladder, following lower spinal cord injury, and performed
retrograde dye analysis to confirm new neuronal pathways that may be created following
nerve transfer. After transection of the spinal roots that provide sensory input to
the urinary bladder, we predicted that restoration of nerve supply (or innervation)
can be achieved by the transfer of a peripheral nerve to a pelvic nerve that is in
close proximity to the bladder, thus bypassing the damaged region and encouraging
nerve regeneration.
What prompted you to pursue research?
My interest in research began when I was a graduate student at Adelphi University
in Garden City, Long Island New York, where I studied pediatric obesity for my Master’s
thesis research project. Following graduation, my interest in research grew, and I
found myself fortunate enough to be selected by Dr. Ruggieri and Dr. Barbe as a research
technician in their lab. I could never have imagined being a part of such a unique
research experience. I developed a new perspective about how research can be applied
to clinical medicine, and how some of our findings could potentially change the lives
of my future patients.
What experience do you have with conducting research?
Using the canine model, we induced a lower spinal cord injury by transecting all sensory
(dorsal) and motor (ventral) nerve roots of the sacral spinal cord that provide innervation
to the urinary bladder. This was done with the use of anesthesia, analgesics and antibiotics.
After 12 months, we began the reinnervation procedure in two phases. Phase one was
an obturator nerve-to-pelvic plexus nerve transfer. We identified an anterior vesical
branch of the pelvic nerve between the bladder and the pelvic plexus that evoked the
largest bladder contraction when stimulated with a bipolar or monopolar probe electrode.
We then joined this nerve, via an end-to-end anastomosis, with a bifurcated portion
of the obturator nerve, which is a lumbar-originating, somatic, sensory and motor
nerve that lies inferior to the urinary bladder.
After one month, we began phase two of the reinnervation procedure. This consisted
of a semimembranosus/semitendinosus branch of the sciatic nerve-to-pudendal nerve
transfer. The sciatic nerve is a motor and sensory nerve with many branches to the
lower extremity. It arises from the lower lumbar and upper sacral segments of the
spinal cord. The pudendal nerve arises from the anterior division of the sacral plexus
and is mainly responsible for sensation and motor innervation of various pelvic muscles
associated with urinary continence. Transferred donor nerves were joined via an end-to-end
anastomosis method to the recipient nerve.
One month post-surgery, we evaluated the functionality of our nerve transfer using
urodynamic testing to determine how well the bladder was storing and releasing urine.
The success of our nerve transfer has yet to be determined in our latest models, but
we will continue to consider this as a main target point of our study.
Additional procedures performed included retrograde dye analyses, which allowed us
to trace axons from the urinary bladder to the spinal cord and dorsal root ganglia,
post-mortem. We also performed smooth muscle strip physiology, post-mortem, where
we are able to test the response of the urinary bladder smooth muscle to various drugs
and electrical stimulation.
What were your responsibilities in your research project?
As a former member of the lab, I was fortunate to be able to participate in numerous
surgical procedures. During the surgeries, I functioned as an anesthesia technician,
a surgical scrub nurse, and as an assistant during the procedures, often helping to
close the spinal and abdominal incisions. Following surgery, I was responsible for
providing all post-operative care and treatments. This included daily vital signs,
wound treatment, physical therapy, and administration of medications. In the lab,
I was responsible for frozen tissue sectioning of previously fixated tissue, as well
as microscope analysis of retrograde dyes using fluorescent microscopy. For the muscle
strip physiology, I often aid with preparation as well as execution of the various
experiments.
What is the broader impact of your research?
It has been estimated that there are approximately 285,000 persons in the U.S living
with a spinal cord injury (SCI) as of 2017, with about 17,500 new SCI cases occurring
each year. Our study focuses primarily on the lower spinal cord, specifically involving
neurogenic bladder. The leading cause of injury is due to vehicular crash, however,
falls, acts of violence and sports/recreational activities also contribute significantly
(The National Spinal Cord Injury and Statistical Center, 2017).
Various diseases such as spina bifida and tethered spinal cord syndrome in children
can also affect the lower spinal cord. Lower spinal cord injury or deficit can result
in weakness and numbness of the lower extremities, sexual dysfunction, spasticity
and exaggerated reflexes, as well as a total loss of bladder and bowel control. Losing
the ability to perform the daily activities of living, as well as experiencing a generalized
loss of independence, can have a devastating emotional and psychological impact on
the affected persons’ life.
The goal of our study is to develop a surgical approach to reinnervate the bladder
so that patients suffering from bladder and bowel incontinence, specifically, can
regain control. We hope that our study will one day be clinically applicable to patients,
and will open the door for future studies involving nerve transfer and axon regeneration.
You May Also Like:
About Philadelphia College of Osteopathic Medicine
Established in 1899, Philadelphia College of Osteopathic Medicine (PCOM) has trained
thousands of highly competent, caring physicians, health practitioners and behavioral
scientists who practice a “whole person” approach to care—treating people, not just
symptoms. PCOM, a private, not-for-profit accredited institution of higher education,
operates three campuses (PCOM, PCOM Georgia and PCOM South Georgia) and offers doctoral degrees in clinical psychology, educational psychology, osteopathic
medicine, pharmacy, physical therapy, and school psychology. The college also offers
graduate degrees in applied behavior analysis, applied positive psychology, biomedical
sciences, forensic medicine, medical laboratory science, mental health counseling,
physician assistant studies, and school psychology. PCOM students learn the importance
of health promotion, research, education and service to the community. Through its
community-based Healthcare Centers, PCOM provides care to medically underserved populations.
For more information, visit pcom.edu or call 215-871-6100.
Contact Us
For general media inquiries, please contact the Office of Marketing and Communications
at 215-871-6300 or communications@pcom.edu. Visit our media relations page to view contact information for public relations personnel.
Connect with PCOM